Home <Services < Cardiology < Postural Tachycardia Syndrome
Postural Tachycardia Syndrome
What is Postural Tachycardia Syndrome (POTS)?
Postural tachycardia syndrome is an abnormal response by the autonomic or involuntary nervous system to standing up.
To be diagnosed with POTS, an individual must experience BOTH of the following:
- A group of symptoms in an upright position (usually standing) that are relieved by lying down
- These symptoms should be associated with an abnormally high and persistent increase in heart rate off 30 beats per minute (40 ppm if under 19 years of age) within 10 minutes of standing
Although symptoms are similar to those experienced by people with abnormally low blood pressure (BP), blood pressure does not usually drop in POTS
POTS can develop in a number of diseases or situations. The reason for this is not properly understood but it is possible that there is a malfunction of the nervous system that controls autonomic functions in the body.
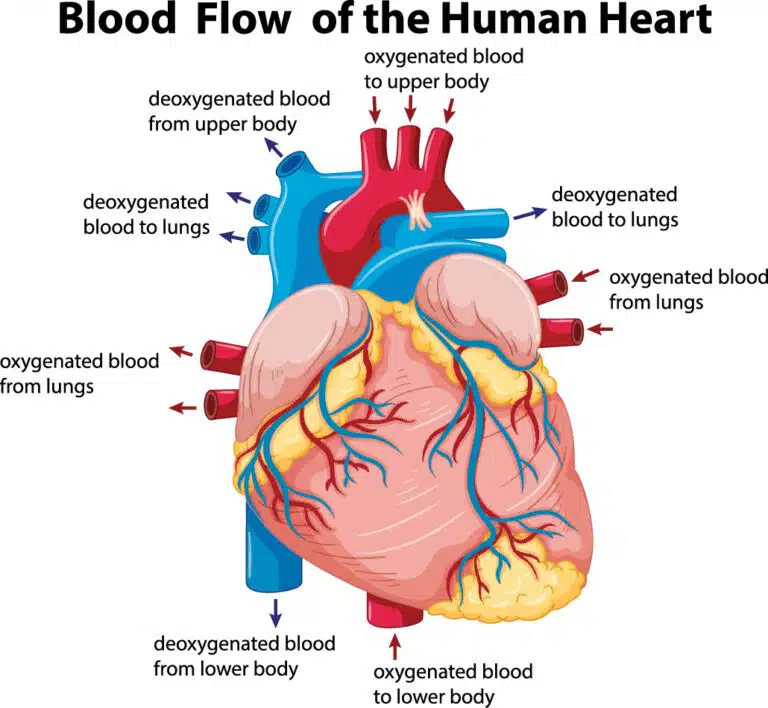
When a healthy person stands up, to avoid blood dropping down to the limbs and abdominal cavity, blood vessels contract immediately and heart rate increases slightly to maintain blood supply to the heart and brain.
In POTS, this automatic adjustment to standing does not work correctly resulting in an excessive rise in heart rate, increased epinephrine in the blood and altered blood flow to the brain.
POTS is more common in women and between the ages of 13 to 50 years.
What are the symptoms of POTS?
The hallmark of POTS is orthostatic intolerance which means that patients experience symptoms when they adopt an upright posture. Symptoms can be very debilitating and range from mild to severe and varying from day to day.
POTS symptoms include:
- Dizziness or near-fainting
- Syncope (fainting)
- Palpitations (an abnormal awareness of heart beat)
- Headaches (which may be more noticeable on adopting an upright posture) or migraine
- Brain fog (difficulty thinking/mental cloudinesss)
- Tiredness
- Sense of anxiety
- Shakiness
- Visual problems (greying, tunnel or glare)
- Gut problems (nausea, diarrhoea, pain)
- Sweating
- Chest pain
- Poor sleep
- Purplish discolouration of skin due to blood pooling in hands and feet
- Bladder problems
What are the triggers for POTS?
For may patients there are certain triggers that seem to make their symptoms worse. Common triggers include:
- Excessive heat
- After eating – especially refined carbohydrates (sugar, white flour etc)
- Standing up quickly
- Dehydration
- Time of day (especially rising after wakening)
- Menstrual period
- Deconditioning or prolonged bed rest
- Alcohol (as it dilates blood vessels)
- Inappropriately excessive exercise
- Temporarily during illness such as viral infections or after operations.
What causes POTS?
There are a number of factors and disorders causing or associated with the condition. In some cases a cause is never identified. POTS can follow a viral illness such as glandular fever, or be linked to pregnancy or a traumatic event. Sometimes teenagers are affected after a rapid growth spurt and most will improve after a few years. Some patients will develop POTS-like symptoms due to a lack of fitness and heart pumping inefficiently after being confined to bed for some time.
Can POTS be mistaken for another condition?
POTS was first recognised by medical journals in 1993. Unfortunately many medical professionals are still unaware of the condition today. Obtaining the right diagnosis can be frustrating and lengthy process. Patients are often misdiagnosed with other conditions such as anxiety and depression, reflex syncope (vasovagal syncope) and chronic fatigue syndrome.

